Converting From Paper To Electronic Medical Records
Posted by admin & filed under EHR, Health Informatics, patient care, healthcare technology, electronic health record, digital medical files.
For years doctors have used paper charts to keep track of patient medical records. While this system may be suitable for small practices, it doesn’t take advantage of technological advances, nor does it facilitate easy sharing of information between medical practices.
The good news is that improvements to the system are already underway thanks to digital upgrades, such as electronic health records (EHRs). For practices interested in improving records storage and integration with online databases that ensure information sharing for better patient care, here’s a basic primer on what electronic medical record implementation entails and how it can best be accomplished.
What is Electronic Medical Record Implementation?
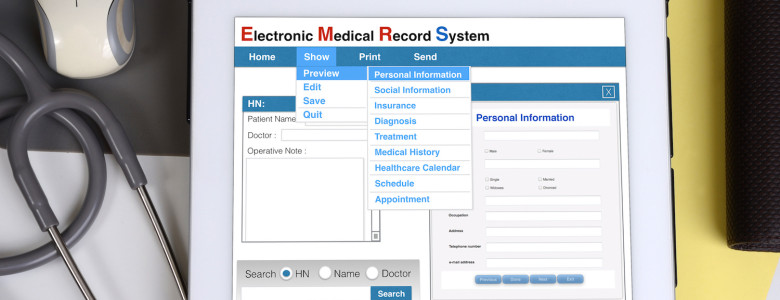
Electronic health records (EHR), on the most basic level, are simply digital versions of standard paper medical records. They are maintained and added to over time by healthcare providers, and they contain medical history, including dates of visit, test results, diagnoses, treatment plans, and more.
What they can do that old-school medical records cannot is share information instantly. Because the records are stored in digital format in an EHR system, parties that are granted access may view patient medical records at any time.
These parties could include any number of private physicians, hospitals and emergency care providers, and of course, patients themselves. This allows all of a patient’s healthcare providers to add information to the records, increasing coordination and reducing overlap. The patient, too, can use these records to gain information and participate in his or her own health and wellness.
Benefits of Upgrading
When you commit to converting paper to electronic health records, medical practitioners can experience a variety of benefits. One of the greatest benefits of converting from paper to electronic health records is ease of access, followed closely by the ability to coordinate care among a number of healthcare providers.
Suppose, for example, that a patient goes to the ER with stomach pain because their primary healthcare provider is off the clock. ER doctors could potentially access medical records to discover that the patient suffers from Crohn’s disease, helping to inform their diagnosis and treatment.
If the patient then visits a primary physician after the fact, the doctor can access records added by ER healthcare providers to see the results of any tests performed and learn what treatments were administered. This level of information sharing allows for coordination of care that is only to the benefit of the patient.
Converting from paper to electronic medical records also increases efficiency, decreases costs, and improves patient care overall. In addition, they could pave the way for a level of self-directed care, or at least at-home monitoring, that makes it easier for patients to manage illnesses and chronic conditions. The potential for good is almost unlimited.
Planning
Now that you understand what EHRs are and how they benefit the medical industry, your next step is to figure out how to implement your own system of electronic medical records. The process begins by assessing your current needs, considering goals, researching available technologies (and how they will integrate with your current system), and seeing how upgrades fit into your budget.
Choosing a System
There are many hardware and software solutions to choose from when it comes to electronic health record implementation, but you want to choose a system that allows for the most coverage in your area. This means checking with local hospitals and other healthcare providers to see what they’re using.
It’s important to select an EHR system that is prevalent among doctors and hospitals you interact with frequently. In addition, you need to make sure that your system is in compliance with all laws relating to healthcare services and patient protection.
Implementation
Once you’ve chosen a system that is suitable for your practice, all that remains is to install it and learn how to use it. Training and testing must occur before the system goes live. Over time you can monitor the system, compile data, and perform audits designed to assess benefits, spot issues, and improve efficiency in order to provide optimal care for patients.